Cure Addiction Now (CAN) is dedicated to the understanding, treatment and ultimate cure of drug addiction. Funding basic research and its clinical translation through a collaborative program is the core focus of the foundation. In addition to creating new therapies to help stop the deadly cycle of addiction, we hope to eliminate the negative stigma of this disease and ultimately find a cure for the brain’s addiction to drugs.
Background:
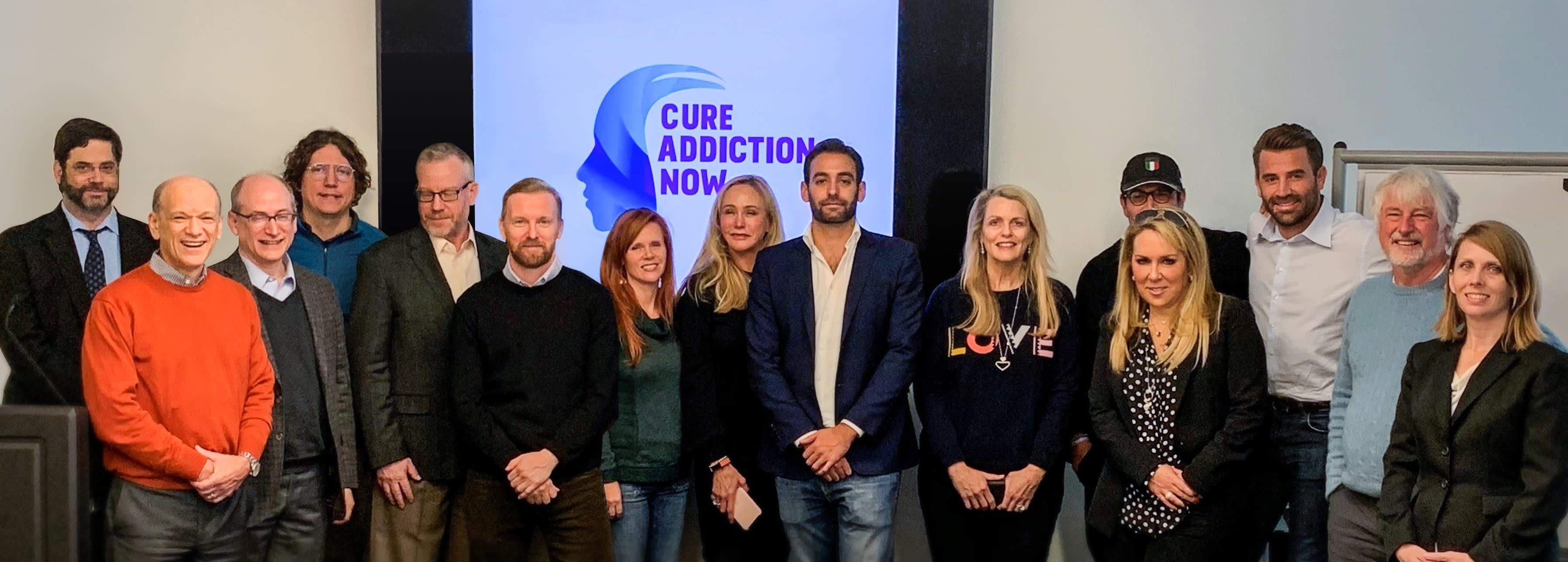
Nancy Davis founded CAN in 2018 with her son Jason Davis who tragically passed away in 2020. Jason’s dream was to fund ground-breaking research to find therapies to help stop the vicious cycle of substance use disorder (SUD) and help people not only detox but stay in permanent recovery. CAN also has plans to fund educational campaigns to remove the negative stigma of SUD and change the narrative. Our mission is to cure addiction now.
At the beginning of Covid 19, one person in the US would die every 11 minutes of an opioid overdose. That number has multiplied dramatically to one person every minute and a half and this does not include other drug overdoses. 70 percent of all deaths are now caused by Fentanyl. Yes, addiction is a real disease and needs to be treated. There is no other disease claiming so many lives. We need to take the stigma of shame away that addicts suffer and treat them with dignity, kindness and compassion the same way we treat everybody else suffering from any disease. We need to raise important funds for our brilliant doctors that represent Mount Sinai, Harvard, UCLA, Scripps, University of Washington and Johns Hopkins and start saving lives. Please Visit our website for more information and a detailed list of our esteemed Scientific Advisory Board and Collaborating Scientists. Below are the currently funded grants from this year. Thank you for your consideration and support!
2021 Grant Awardees: Research Progress Report as of 10/1/2021
Research Project #1: Developing a Strategy to Prevent Relapse to Opioid, Nicotine,
Alcohol and Cocaine Use with a Single Use Medication
Courtney A. Miller, PhD, Scripps Research
Substance use disorder (SUD) is a chronic, relapsing disorder with a severe lack of treatment options. Associations that have formed during periods of drug use serve as powerful relapse factors by triggering motivation to seek the drug. Recently, we identified the molecular ATPase and driver of synaptic actin polymerization, nonmuscle myosin II (NMII), as a biological target for the selective disruption of these associations. A single treatment with the NMII inhibitor Blebbistatin (Blebb) produces an immediate, seemingly permanent loss of motivation for methamphetamine (METH) and amphetamine (e.g. Adderall) by targeting the associated memories. This occurs without the need for retrieval and without affecting other types of memories, including those associated with other drugs of abuse. In addition to its efficacy in animal relapse models following a single treatment, several properties made Blebb an excellent starting point for medication development. Paramount among these are the molecule’s high brain penetration (thus, lower doses can be used) and rapid clearance from the body and brain (limiting unwanted peripheral and central effects on the body). Unfortunately, Blebb’s activity at cardiac muscle myosin II (CMMII), a protein critical for heart function, was a liability. Through work funded by the NIH, including NIDA, we have developed a preclinical candidate compound, MT-110, that retains Blebb’s high brain penetrance and rapid clearance, but no longer inhibits CMMII. The result is a dramatically improved safety profile and a therapeutic index (ratio of the lowest dose that achieves the desired effect and the highest tolerable dose) of at least 25x. We have filed a non-provisional patent in the US and ten other countries, declared a preclinical candidate, and are now preparing to file an IND with FDA and designing our first in human Phase 1 trial. Recognizing that it would be powerful to utilize the Blebb-based NMII inhibitor to target motivation for other widely used drugs of abuse, particularly opioids, alcohol, nicotine and cocaine, we have begun working on a strategy. Blebb disrupts restabilization of these memories when animals are exposed to reminders associated with the drug of abuse. However, for individuals that use drugs, associations capable of motivating drug seeking can number in the hundreds and even be unconscious motivators. Therefore, it is not feasible for subjects to actively retrieve all “triggers” in a clinical setting for reconsolidation targeting. Interestingly, recent evidence in animal and human studies indicates a similar disruption can be achieved by pairing a reconsolidation disrupting intervention with a small amount of the drug of abuse itself. We now have promising preliminary preclinical data using this strategy that points to the potential for MT-110 in cocaine, nicotine and opioid use disorders. Additional studies to validate and extend these findings are underway.
Research Project #2:
Role of chemosensory processing in choroid plexus circuit in drug addiction
Paul J. Kenny, Ph.D. and Stephanie P.B. Caligiuri, M.D., Mount Sinai, New York
Sensitivity to the aversive properties of addictive drugs influences vulnerability to substance use disorders (SUDs). Indeed, aversive reactions to drugs of abuse upon their first usage decreases the likelihood that subsequent use will transition from occasional to habitual. Little is known about the mechanisms of drug aversion. Taste systems guide ingestive behaviors to ensure survival by detecting sweet, salty, & umami flavors, which represent carbohydrates, electrolytes, and protein respectively. Taste systems also detect sour and bitter tastes, which often reflects spoiled or poisonous substances. Intriguingly, most addictive drugs are bitter-tasting plant-derived alkaloids, a class of compounds known to activate taste-2 receptors (T2Rs). In addition to their abundant expression in the oral cavity, accumulating evidence suggest that T2Rs are also expressed outside the oral cavity. Individuals carrying genetic variation in genes that encode components of the T2Rs and related signaling machineries are at increased risk of developing SUDs. With the support of Cure Addiction Now (CAN), we are testing the hypothesis that oral and/or extra-oral T2Rs are activated by opioids and other classes of addictive drugs, and that this action contributes to their aversive properties that protect against SUDs. Using genome editing technologies and cellular assays of T2R function, we have collected compelling data suggesting that drugs of abuse stimulate T2R signaling. We have also shown that the same neurons in brain aversion centers that are activated by consumption of noxious bitter compounds such as quinine are also recruited by drugs of abuse. Moreover, we have shown that genetic manipulations that selectively perturb T2R signaling attenuated aversive responses to drugs of abuse and increases their consumption. Perhaps most surprisingly, we found that T2R-mediated aversive sensory information related to drugs of abuse is routed to the choroid plexus in the fourth ventricle, a secretory organ in the brain, and that manipulating genes in the choroid plexus regulates aversive behavioral responses to addictive drugs. These data reveal a novel chemosensory mechanism that regulates addiction-relevant behavioral responses to drugs of abuse that may serve as a substrate for the development of target therapeutics for SUDs.
Research Project #3
The Kappa Opioid Receptor: A Therapeutic Target for Negative Affect in Pain and Addiction
Catherine Cahill, Ph.D. and Edythe London, Ph.D., UCLA
Anhedonia is the impaired capacity to experience pleasure from naturally rewarding objects and events. It is defined as a state of ‘markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day’. While it is relatively undertreated, it occurs in many neuropsychiatric disorders including substance use disorders and chronic pain. Considering the high comorbidity between negative affective states, such as depression and chronic pain, it is not surprising that anhedonia may be a driver of opioid addiction, where opioid misuse is a predictor of anhedonia.
Kappa opioid receptor agonists produce dysphoria, depressive-like symptoms and psychotomimetic effects in humans, and they elicit aversion and depressive-like behaviors in preclinical models. A novel kappa receptor antagonist JNJ-67953964 produced anti-anhedonic effects in a recent, multicenter, double-blind, placebo-controlled, randomized clinical trial. Given the involvement of this receptor in negative affective states and the positive preliminary clinical study in alleviating anhedonia, our studies focus on kappa receptors with the goal of facilitating the development of medications for Opioid Use Disorder.
Our first aim was to determine the association of kappa binding in limbic regions of brain with measures of negative affect in a model of chronic pain. To date, we have demonstrated kappa receptor binding in the striatum using microPET and 18F]LY2459989, a novel kappa radiotracer. Binding of this tracer was blocked by both a kappa-receptor selective antagonist the nonselective opioid antagonist naloxone. We have also conducted longitudinal studies were animals were imaged over time to correlate changes in receptor binding with the development of negative affective states. Analysis of these data are ongoing.
Studies in people who misuse heroin show that acute opioid withdrawal increases opioid craving and seeking behavior, and that the severity of withdrawal predicts the response to treatment. We therefore have conducted microPET imaging in opioid-dependent rats during the acute phase of opioid withdrawal. Analysis of these studies are ongoing.
Donors
Jennifer Marquez I gave a donation as a means for my extended family to honor my mom, Yvonne Parsons, my brother, Zach Parsons, and my cousin, Justin Locke this holiday season. These are three of our loved ones whose lives were cut short due to substance ab...
